An interview with Dr Matthew Reid [Sleep Researcher and Assistant Professor of Psychiatry at Johns Hopkins School of Medicine]
By Dr Anna Weighall, Sleep Researcher and Reader in Psychology and Education, University of Sheffield
I spoke to Dr Matthew Reid - an Assistant Professor of Psychiatry with a background in neurology, currently working at Johns Hopkins School of Medicine, and previously of the Sleep & Circadian Neurosciences Institute, at the University of Oxford. Matthew focuses on understanding the neurological and psychological consequences of poor sleep, including insomnia, chronic sleep disruption, and acute sleep deprivation. His research explores the complex interrelationship between sleep and mental health, with a current emphasis on how sleep disruption affects sensitivity to mood and pain through large-scale laboratory and treatment studies.
1. What initially sparked your interest in the field of sleep research
It’s not unusual to hear of people getting into sleep by accident, and I guess for me it all started with a bit of a ‘wrong place, right time’ kind of situation when I was a student at University of Sheffield. At the time I was studying neurology at the medical school and accidentally showed up at the wrong clinic observation one day. Obviously, it didn’t take long to realise that what I thought was an epilepsy clinic was actually an excellent sleep-neurology clinic run by Dr Gary Dennis. I was so interested by the patients stories I just kept coming back. That, plus enduring the misery of rotating nightshifts in hospitals and sleep labs ultimately drove me away from the idea of wanting to be a doctor and instead decided to pursue a career in sleep research. I eventually ended up doing a PhD with Simon Kyle and Colin Espie at the University of Oxford which pulled me in even deeper and the rest is obviously history.
2. Can you tell us more about the work being conducted in your sleep lab at Johns Hopkins?
I work in the US at the moment, and we’re fortunate enough to have access to some amazing funding resources the enable us to do some really interesting and innovative studies. Most of my ongoing studies involve some aspect of investigating the effects of sleep loss on mental health, but we’ve been especially fortunate enough to obtain over $10mn of funding from the US government to study to the effects of experimental sleep deprivation on opioid use and addiction. We are trying to understand whether having poor sleep, or having your sleep disrupted by environmental circumstances affects the way that opioids work inside the brain, and whether that increases your chances of become addicted to opioids. We already have some data to suggest that is the case, but the two ongoing studies in our sleep lab will really provide some fundamental evidence to answer those questions.
3. What kind of methodologies do you use in your studies?
At the moment we’re recruiting healthy individuals, and individuals with chronic pain disorders who rather admirably agree to being sleep deprived, or having their sleep disrupted in the sleep laboratory for four days! Some of them are woken up several times throughout the night, some of them are disrupted by noises and vibrations that we play every time they go into slow wave sleep. It’s really brutal stuff, so I always admire the participants who want to help out with our research. If that doesn’t sound rough enough, each daytime after they are sleep deprived, we then subject them to a bunch of pain testing, and put them in the PET scanner whilst injecting them with high doses of carefully administered opioids to examine whether sleep deprivation alters the way the drug binds to opioid receptors in the brain.
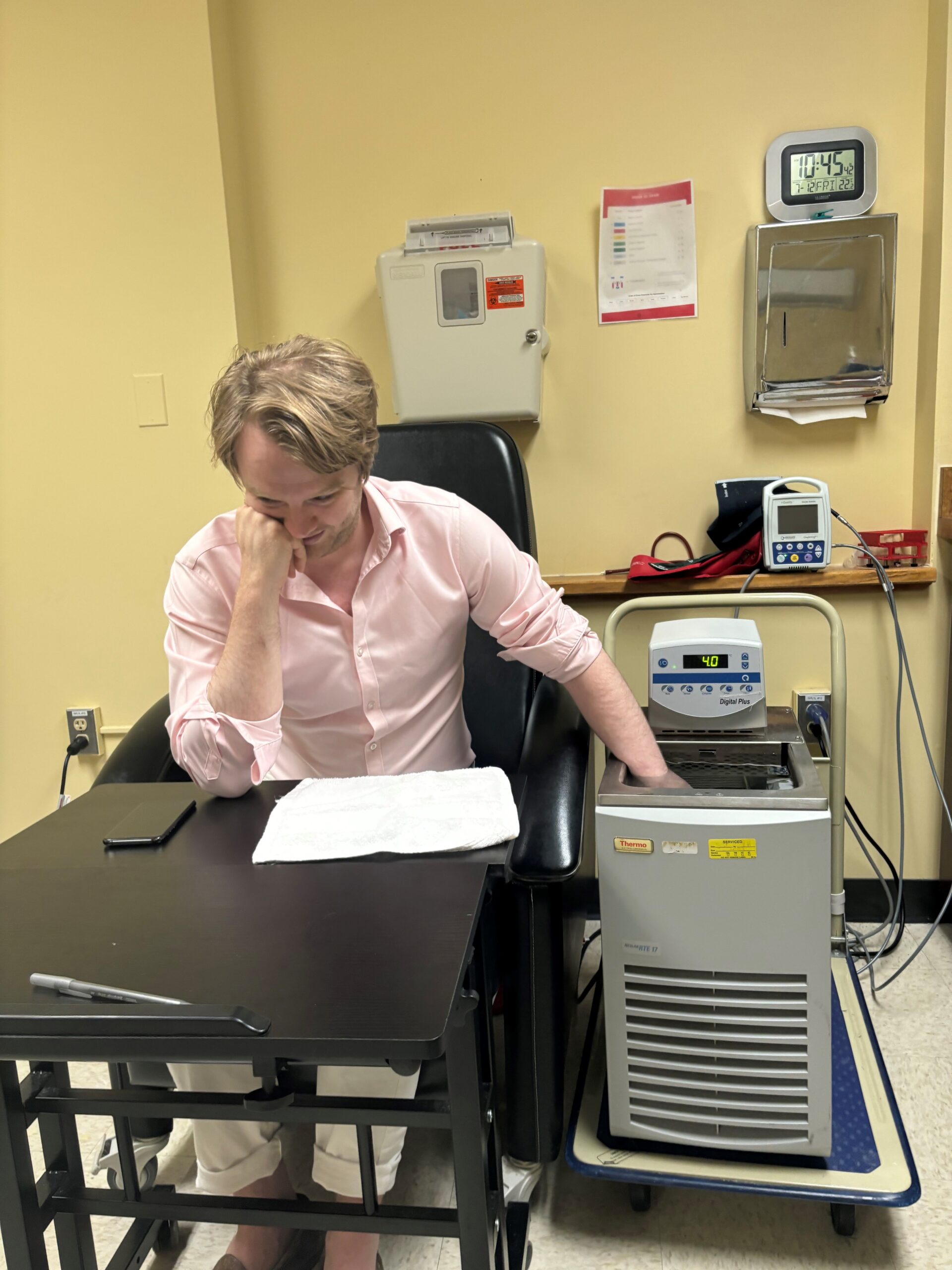
The pain testing is quite interesting. We put them through a battery of tests known as ‘Quantitative Sensory Testing’ which assess both pain tolerance (how much pain can they handle) as we as pain threshold (When do they begin to perceive pain) using lots of different types of stimuli. The ones people seem to enjoy least is the cold-pressor test : Where they have to keep their hand in a chamber of water which is constantly maintained at 4c (just above freezing) for up to five minutes. It doesn’t sound that bad, but it REALLY hurts. I tried it out this morning when I was training some of our students, and I almost felt like I was going to throw up. At the same time we do other pain testing (such as administering a hot thermal probe) to see if one type of pain interferes with the perception of another – to study a really interesting phenomenon called ‘conditioned pain modulation’.
4. What role do you think emerging technologies, such as wearable sleep trackers or advanced imaging techniques, will play in the future of sleep research?
The biggest shift in my field over the past 5-10 years has been a mass migration from in-lab Polysomnography to at-home wireless Sleep-EEG devices. I feel like each time I go to a sleep conference there’s a dozen new devices that I hadn’t even heard of before. The field is moving really quick. I was very sceptical of these devices at first, but now I’ve more or less changed to using them entirely. Obviously, there’s a big trade off between data-quality and convenience, but the ability to record in patients own homes and do so at a huge scale is a real game changer. There’s always been a catch 22 type situation with sleep research – the effect of sleep physiology you try to observe are small, so we need large studies, but getting anything more than 20 or 30 people into the sleep lab has been huge and expensive effort. In the end, most studies end up using the same sample sizes and come to the same conclusion that “bigger studies with greater power are needed”, but we haven’t had a way of getting round that problem. I think we’re going to see a gradual shift in the size of a ‘typical’ sleep study as more people start to use these devices. We’re already seeing that shift towards ‘Big-Data’ through initiatives such as the National Sleep Studies Resource (NSSR), but low-cost wearables and EEG devices will help accelerate the movement, and will open up a lot of doors in terms of these fundamental but unanswered questions of how sleep physiology impacts physical and mental health.
5. What do you see as the most pressing questions or challenges in this field that need to be addressed in the coming years?
As we’ve just alluded to, it’s becoming easier and easier to measure sleep. Which is a great thing, but that brings its own challenges. What was once a tool reserved for a small portion of highly skilled individuals is now accessible to more or less anybody with an interest in sleep and the money to pay for a device. Not only does that mean there are more people doing sleep research, but more companies trying to profit off the industry. This commoditisation of sleep data by commercial entities is a little troubling, as the increasing levels of obfuscation are pushing researchers further and further away from the raw data, and from being able to produce truly reproducible science. A great example of this is what happened with the dreem EEG headbands when they were bought out by Beacon Biosignals, and all of a sudden everyone using the devices was asked to pay >£100k just to carry on using the devices. I can’t help but feel we are becoming a little bit too dependent on these kinds of Black-Box devices. Wireless EEG and wearables are great, but we need more tools that are geared towards researchers rather than consumers. As scientists, we need to know everything about the equipment we use as well as if and how it modifies the data we collect. I may be a little biased here because I’ve been working with some brilliant engineers in the applied physics laboratory at Hopkins, and we are in the process of releasing our own fully open-source wireless EEG device designed for research. Okay, I’m very biased, but the whole point is we are building a device that can be constructed very cheaply (~$100) by anybody based on some free instructions we are releasing on the internet, so I don’t really stand to gain anything. The plans and all the source code will be 100% open source for people to do what they want with.